
Compassionate care for your mind, body, and soul, every day
Health care refers to the maintenance and improvement of physical, mental, and emotional well-being through the prevention, diagnosis, treatment, and management of illness, injury, and disease. It encompasses a wide range of services provided by healthcare professionals, including doctors, nurses, therapists, and other healthcare practitioners.
WE OFFER A VARIETY OF SOLUTIONS
Our Treatment

Infertility treatment refers to medical interventions designed to help couples or individuals who are unable to conceive naturally. Infertility affects millions of people worldwide, and can result from a variety of factors, such as hormonal imbalances, genetic disorders, physical abnormalities, or lifestyle factors.
There are several different types of infertility treatment available, depending on the underlying cause of infertility and the specific needs of the patient. These treatments can include:
- Medications: Certain medications can be prescribed to stimulate ovulation or improve sperm production.
- Intrauterine insemination (IUI): In this procedure, sperm are placed directly into the uterus during ovulation to increase the chances of fertilization.
- Intrauterine insemination (IUI): In this procedure, sperm are placed directly into the uterus during ovulation to increase the chances of fertilization.
- Intracytoplasmic sperm injection (ICSI): This procedure involves injecting a single sperm directly into an egg to facilitate fertilization.
- Donor eggs or sperm: In some cases, individuals or couples may use donated eggs or sperm to conceive.
- Surrogacy: Surrogacy involves using a gestational carrier to carry a fertilized embryo to term.
Infertility treatment can be emotionally and financially challenging, and success rates vary depending on a range of factors. It is important for individuals and couples to work closely with their healthcare providers to determine the most appropriate course of treatment and to receive ongoing support throughout the process.
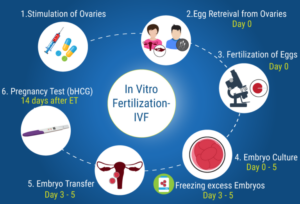
IVF-ET (in vitro fertilization-embryo transfer) is a type of assisted reproductive technology (ART) that is used to treat infertility. It involves fertilizing eggs with sperm in a laboratory dish and then transferring one or more resulting embryos into the uterus of the woman.
The IVF-ET process typically involves several stages:
Ovarian stimulation: Fertility medications are used to stimulate the ovaries to produce multiple eggs.
Egg retrieval: A procedure is performed to retrieve the mature eggs from the ovaries.
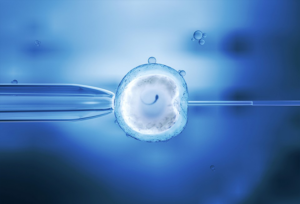
Fertilization: The retrieved eggs are fertilized with sperm in a laboratory dish to create embryos.
Embryo culture: The resulting embryos are cultured in a laboratory for several days to allow them to develop.
Embryo transfer: One or more of the resulting embryos are transferred to the uterus of the woman, typically 3-5 days after fertilization.
Pregnancy testing: About two weeks after the embryo transfer, a pregnancy test is performed to determine if the procedure was successful.
IVF-ET is a complex and often emotionally challenging process, and success rates can vary depending on a range of factors, such as the age of the woman, the quality of the sperm and eggs, and the number of embryos transferred. It is important for individuals and couples considering IVF-ET to work closely with their healthcare providers to determine the most appropriate course of treatment and to receive ongoing support throughout the process.

Cryopreservation of gametes refers to the process of freezing and storing sperm and/or eggs for future use. This technique is often used in assisted reproductive technologies (ART), such as in vitro fertilization (IVF), to increase the chances of successful fertilization and pregnancy.
The process of cryopreservation typically involves the following steps:
Sperm or eggs are collected from the donor through a process called sperm or egg retrieval.
The gametes are mixed with a special solution, or cryoprotectant, which helps to protect them during the freezing process.
The gametes are then frozen and stored in liquid nitrogen at extremely low temperatures (-196°C) until they are needed.
When the gametes are needed, they are thawed and used in an ART procedure, such as IVF.
Cryopreservation of gametes can be beneficial for several reasons. For example, it can allow individuals to preserve their fertility before undergoing medical treatments, such as chemotherapy or radiation, that may damage their reproductive organs. It can also be used by individuals who are not yet ready to start a family, but want to preserve their ability to do so in the future.
While cryopreservation can increase the chances of successful fertilization and pregnancy, success rates can vary depending on a range of factors, such as the quality of the gametes and the age of the donor. It is important for individuals considering cryopreservation to work closely with their healthcare providers to determine the most appropriate course of treatment and to receive ongoing support throughout the process.

Embryo fertility enhancing and fertility preserving endoscopy are minimally invasive surgical techniques used to diagnose and treat infertility in women. These procedures are typically performed by a reproductive endocrinologist and can help to identify and address issues that may be preventing pregnancy.
Embryo fertility enhancing endoscopy involves the use of a small camera, called a hysteroscope, to examine the inside of the uterus and fallopian tubes. This procedure can help to identify and remove any polyps, fibroids, or other abnormalities that may be interfering with implantation or fertility.
Fertility preserving endoscopy involves the use of a laparoscope, a small camera inserted through a small incision in the abdomen, to examine the reproductive organs and identify any issues that may be affecting fertility. This can include endometriosis, ovarian cysts, or blocked fallopian tubes.
In some cases, these procedures may also involve the use of lasers or other tools to remove or repair any identified issues. By addressing these issues, embryo fertility enhancing and fertility preserving endoscopy can help to improve the chances of successful pregnancy and childbirth.
However, it is important to note that these procedures are not appropriate for all individuals and may not always be successful. It is important for individuals considering these procedures to work closely with their healthcare providers to determine the most appropriate course of treatment and to receive ongoing support throughout the process.

Laparoscopic and endoscopic surgery are minimally invasive surgical techniques that use small incisions and specialized tools to access and treat various conditions within the body. Both techniques can offer benefits over traditional open surgery, such as less pain, reduced recovery time, and a lower risk of complications.
Laparoscopic surgery involves making small incisions in the abdomen and inserting a laparoscope, a thin tube with a camera and light, to visualize the internal organs. The surgeon can then use specialized tools to perform the procedure, such as removing an inflamed appendix or repairing a hernia.
Endoscopic surgery, on the other hand, involves using an endoscope, a flexible tube with a camera and light, to examine and treat the inside of the body through natural orifices, such as the mouth or anus. This technique is often used to diagnose and treat conditions such as ulcers, polyps, or tumors in the digestive tract.
Both laparoscopic and endoscopic surgery offer several advantages over traditional open surgery, including smaller incisions, less pain, reduced scarring, shorter hospital stays, and faster recovery times. Additionally, these procedures are generally associated with lower rates of complications and infections.
However, these techniques are not appropriate for all surgical procedures or all individuals. It is important to work closely with a healthcare provider to determine the most appropriate course of treatment for a particular condition.
Intracytoplasmic sperm injection (ICSI) and embryo transfer (ET) are two related techniques used in assisted reproductive technologies (ART) to treat infertility.
ICSI is a specialized form of in vitro fertilization (IVF) in which a single sperm is injected directly into an egg using a fine needle. This technique is typically used when there are issues with sperm quality or quantity, such as low sperm count or motility. ICSI can increase the chances of successful fertilization and pregnancy, even in cases of severe male infertility.
Once the eggs have been fertilized through ICSI, they are cultured in a laboratory for several days before being transferred into the uterus through ET. Embryo transfer is a key component of the IVF process and involves placing one or more embryos into the uterus using a thin catheter. The goal of ET is to maximize the chances of successful implantation and pregnancy.
ICSI-ET is the combination of these two techniques, in which the fertilized eggs are transferred into the uterus after being created through ICSI. This technique can be beneficial for individuals and couples who have struggled with infertility due to male factor infertility, such as low sperm count or motility.
While ICSI-ET can increase the chances of successful pregnancy, it is important to note that success rates can vary depending on a range of factors, such as the age and health of the individuals involved. It is important for individuals considering ICSI-ET to work closely with their healthcare providers to determine the most appropriate course of treatment and to receive ongoing support throughout the process.
